
Dr Rob Hicks
http://www.bbc.co.uk/health/conditions/ptsd1.shtml
The symptoms of post-traumatic stress disorder usually develop within three months of a traumatic event.
For many people, post-traumatic stress disorder (PTSD) conjures up images of Vietnam war veterans. Although their experiences did bring the problem into the spotlight, PTSD was first described more than 100 years ago among people involved in train accidents.
PTSD is now recognised as a debilitating consequence of been involved in, or witnessing alarming events, from natural disasters to sudden unexpected bereavement, or even been diagnosed with a serious illness. However, the greatest risk of PTSD is from violent attacks.
Could you have PTSD?
The symptoms of PTSD usually develop within three months of a traumatic event, although they can take up to a year to appear and must persist for at least a month for it to be diagnosed. There are three main types of symptoms:
Intrusion, the event is constantly revisited in the persons mind:
flashbacks (sudden unwanted vivid memories, such as reliving the event)
painful emotions.
Avoidance:
numbness and loss of deep feelings
depression, guilt and anxiety
retreat from relationships
avoidance of activities that may trigger memories of the event
avoidance of dealing with the grief and anger
avoidance of symptoms by using "self-medication" with alcohol or drugs, problems with drug and alcohol abuse
Increased arousal, the feeling of constant threat can lead to:
very short temper
irritable emotions
anger
difficulty concentrating
disrupted sleep and nightmares
poor mental and work performance
Research
Research is helping to point out specific areas of the brain that are involved in PTSD, particularly in generating the state of anxiety and fear, which is typical of the condition. For example, there is some evidence that an area deep within the brain called the Amygdala, which is thought to control the body's fear response, may be abnormally activated in PTSD.
Other research has found abnormalities in the production of hormones the body creates when stressed, levels of naturally produced opiate chemicals and neurotransmitters - the chemicals that control brain cell activity.
Psychological therapies
People can recover from PTSD within months, but for some the condition can last for many years. Treatment is based on a combination of psychological therapies and medication such as drugs for depression and anxiety.
Cognitive-behavioural therapy can help people understand the condition and thought processes. Through breathing techniques and anger control patients can learn how to change their behaviour or reaction to their symptoms.
Exposure therapy can also be helpful, although it may seem stressful at first as it involves confronting the fears and reliving the event, with the therapist, to help the person learn how to cope.
ABC World News Tonight, MDMA/PTSD feature story
Post-traumatic stress disorder
http://en.wikipedia.org/wiki/Post-traumatic_stress_disorder
http://www.answers.com/topic/posttraumatic-stress-disorder
A psychological disorder affecting individuals who have experienced or witnessed profoundly traumatic events, such as torture, murder, rape, or wartime combat, characterized by recurrent flashbacks of the traumatic event, nightmares, irritability, anxiety, fatigue, forgetfulness, and social withdrawal.
Post-Traumatic Stress Disorder (PTSD) is a psychological condition, affecting people who have experienced an event that involves actual or threatened death or serious injury to themselves, witnessing of horrifying events and feeling unable to escape or alter them, or learning about the violent death or serious injury of a family member or close associate. PTSD can occur at any age, and symptoms usually manifest within three months but might be delayed by years. Features of PTSD include intrusive memories or thoughts about the event, efforts to avoid thinking about the event, a general numbing of emotional responsiveness, and a constantly heightened level of arousal. A diagnosis of PTSD requires that symptoms have been present for at least a month and hamper normal functioning in social and work settings. Dissociation, a sense of detachment from the reality of one's surroundings, is a way people often cope with repeated trauma. PTSD, as the explanation for "hysteria," emerged in the research of French psychologist Pierre Janet and, early in his career, that of Sigmund Freud. During World War I, PTSD, called combat neurosis, shell shock, or battle fatigue, was common in soldiers. The American psychiatrist Abram Kardiner developed this concept in his book The Traumatic Neuroses of War (1941). PTSD became an official diagnosis of the American Psychological Association in 1980, due largely to the symptoms of Vietnam veterans. The revival of the feminist movement in the late 1960s led to heightened awareness of domestic violence and abuse as a cause of PTSD.

Veterans Affairs Urged to Address Care for Veterans With Post-Traumatic Stress Disorder
Tuesday, May 08, 2007
http://www.foxnews.com/story/0,2933,270678,00.html
WASHINGTON — The surge in the number of veterans suffering post-traumatic stress disorder requires development of better tests to evaluate affected personnel and determine how best to compensate them, a panel of medical experts said Tuesday.
"As the increasing number of claims to the VA shows, PTSD has become a very significant public health problem," said Nancy Andreasen, chair of the committee that prepared the report.
"Our review of the current methods for evaluating PTSD disability claims and determining compensation indicates that a comprehensive revision is needed," said Andreasen, head of the psychiatry department at Carver College of Medicine, University of Iowa.
Claims increased from 120,265 in 1999 to 215,871 in 2004 and payments jumped from $1.72 billion to $4.28 billion in the same period, a combined committee from the Institute of Medicine and National Research Council said.
While the largest share of claims is still coming from Vietnam War veterans, there are expected to be many more claims in future from personnel who served in the first Gulf War and in the current conflicts in Iraq and Afghanistan, the panel said.
But the Veterans Affairs Department uses only crude criteria for rating disabilities due to mental illness and is not consistent for relapsing conditions, according to the report, which had been requested by the VA.
The panel urged the VA to develop new criteria based on the diagnostic standards of the American Psychiatric Association and to establish certification programs for workers who deal with PTSD claims.
The panel said the VA should base compensation decisions on how greatly PTSD affects all aspects of a veteran's daily life, not just his or her ability to be gainfully employed.
The report also noted that PTSD can be triggered by trauma other than combat, such as sexual assault. Female veterans are less likely to receive compensation for PTSD, which may in part be due to the difficulty of substantiating exposure to traumatic events unrelated to combat, including sexual harassment or assaults that occurred during service, the report said.
It urged the VA to gather data and provide reference materials to help disability raters better address the management of PTSD claims related to sexual assault during military service.
The Institute of Medicine and National Research Council are branches of the National Academy of Sciences, an independent organization chartered by Congress to advise the government on scientific matters.

Post-Traumatic Stress Disorder Concerns
What Is the Effect of Constant and Widespread Violence on Soldiers in Iraq?
Sgt. John Newport left Iraq months ago, but he is still struggling with what he experienced there. He keeps playing one scene over and over again in his mind.
http://abcnews.go.com/Nightline/story?id=331092&page=1
It took place when he was in his Humvee, passing a convoy of trucks that was hauling tanks. One of the truck drivers tossed a bag of M&Ms at a bunch of Iraqi kids.
A little girl went to pick it up, but there was a truck behind her. The driver didn't see her, and ran her over.
"The hardest part for me is that she was about the same age as my daughter is," Newport told "Nightline," with tears welling up in his eyes. "After that truck had run her over, you couldn't even tell it was a person."
Newport has what doctors call post-traumatic stress disorder, a condition often linked to depression and floating anxiety.
There are concerns that the Iraq war is producing more cases of PTSD than any conflict in decades because the violence has been so widespread and exposure to it so constant over long periods.
Newport says he began reliving the scene when he returned home to the Army base at Ft. Polk, La., and saw his daughter for the first time. "But it was no longer that little Iraqi girl," he said. "That was my daughter going into that road."
One Out of Six May Struggle
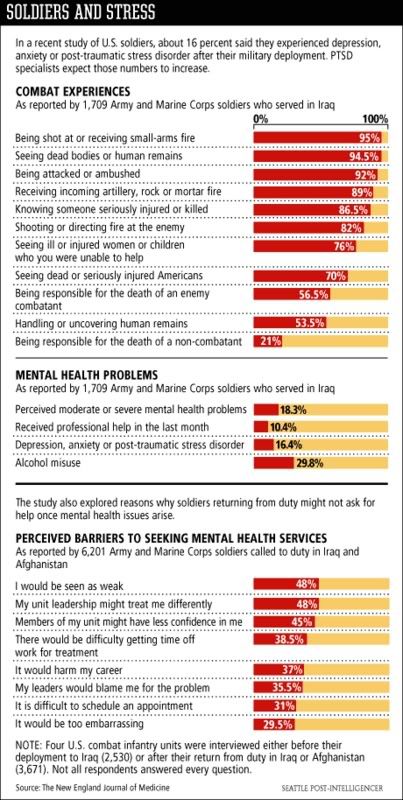
A study published in the New England Journal of Medicine found that one out of six soldiers surveyed may be struggling with PTSD.
More than 300,000 U.S. soldiers have served in Iraq. There are about 140,000 there now.
But the study was done early in the conflict. In many respects things have gotten worse.
"If there's increased threat, if they're more exposed, then there'll be higher rates," said Robert Ursano, director of the Center for Traumatic Stress and chief psychiatrist at the military's own medical school.
Iraq -- with suicide bombers, roadside mines and the constant threat of attack -- poses a unique challenge to the mental health of American soldiers.
"They're more at risk and they feel that risk in an ongoing way," Ursano said. "There's not an area of safety. It's all relative safety. In other wars, one has been able to have spots where, in fact, safety could be relatively ensured. That's less true in Iraq."

Iraq veterans return home to an uncaring population
http://www.mercurynews.com/opinion/ci_5815671
Despite the lack of a clear Iraq mission statement, sol- diers believe they're carrying out an important task.
NEW YORK - Paul Rieckhoff looked across the crowded restaurant, which was not far from Times Square.
"During World War II," he said, "we could be in this place and there would be a guy sitting at that table who was in the war, or the bartender had been in the war. Everybody you saw would have had a stake in the war. But right now you could walk around New York for blocks and not find anybody who has been in Iraq.
"The president can say we're a country at war all he wants. We're not. The military is at war. And the military families are at war. Everybody else is shopping."
Rieckhoff is an imposing 6-foot-2, 245-pound former infantry officer who joined the military after graduating from Amherst College. When he came home from a harrowing tour in Iraq in 2004, he vowed to do what he could to serve the interests of the men and women who have fought in Iraq and Afghanistan but have never fully received the support they deserve from the government or the public at large.
He wrote a book, "Chasing Ghosts," which is now out in paperback, and he formed a powerful veterans' advocacy organization called Iraq and Afghanistan Veterans of America.
Rieckhoff is not bitter. He's actually funny and quite engaging (and a good writer). But he has very little tolerance for the negligence and incompetence the government has shown
in equipping the troops and fighting the war in Iraq, and he is frustrated by the short shrift that he feels the troops get from the media and the vast majority of Americans.
There's a gigantic and extremely disturbing disconnect, he says, between the experiences of the men and women in uniform and the perspective of people here at home. "We have a very diverse membership in IAVA," he said. "We've got Republicans and Democrats and everything in between. But one of the key things we all have in common is this frustration with the detachment that we see all around us, this idea that we're at war and everybody else is watching `American Idol.'
"I think that's one of the main reasons why so many guys want to go back to Iraq. They come home and feel like: `Man, I don't fit in here. You know, I'm out of place.'" Even though there's never been a clear statement of the military's mission in Iraq, and the goals have shifted from month to month and year to year, the soldiers and Marines who have been sent there have felt that they were carrying out an important task on behalf of the nation.
"It's tough to have such a serious sense of commitment," Rieckhoff said, "and then come home and see so many people focused on such frivolous things. So I think that frustration is serious and growing. And I'll tell you the truth: I blame the president for that. One of the biggest criticisms of the president, and I hear this across the board, is that he hasn't asked the American people to do anything."
Rieckhoff is convinced that if the public heard more from the soldiers and Marines who have actually experienced combat, including those who have been wounded and suffered emotional trauma, the wars in Iraq and Afghanistan would be viewed more seriously. Part of the problem, he said, is that too many civilians have little or no understanding of what war is really like, and of the toll it takes beyond the obvious toll of the dead and wounded.
Among other things, there are family problems, drug and alcohol abuse, untreated post-traumatic stress disorder, depression and suicide - all directly attributable to service in a war zone. "Incredibly," he writes in his book, "no government agency keeps track of the number of veterans who kill themselves after their service has ended - another sign of how little value is placed on veterans' long-term well-being."
I mentioned a young soldier I had interviewed in 2005 who worried that because he had killed three insurgents during a battle in Iraq he might not be "allowed into heaven." The soldier wondered whether he had "done the right thing."
Rieckhoff nodded. "Asking somebody to die for their country might not be the biggest thing you can ask," he said. "Asking my guys to kill - on my orders, as an officer - that's difficult. I'm telling that kid to squeeze that round off and take a man's life. And then he's got that baggage for the rest of his life. That's what you have to live with."
I signaled for the check, and we left the restaurant. It was a beautiful, sunlit afternoon. New Yorkers were smiling and enjoying the spring weather. There was no sign of a war anywhere.
BOB HERBERT is a columnist for the New York Times.
Soldiers with Post Traumatic Stress Disorder
Combat stress has Pentagon under siege
http://www.chieftain.com/metro/1178514141/1
Combat stress reviews show that troops are reluctant to ask for mental health care.
By PETER ROPER
THE PUEBLO CHIEFTAIN
As the war in Iraq enters its fifth year, the Pentagon is under siege from within and without over how it handles the growing numbers of soldiers and Marines suffering from combat stress.
Only last Thursday, the Defense Department's Task Force on Mental Health delivered its preliminary report that said 38 percent of soldiers and 31 percent of Marines report mental health issues ranging from post-combat stress to severe brain injuries - and those numbers are likely to worsen as troops return to Iraq for multiple deployments.
The numbers are even worse for the part-time soldiers who have been fighting in Iraq, members of the National Guard. The task force found that nearly 50 percent of Guard members reported mental health issues after deployment.
"The system of care for psychological health that has evolved in recent decades is not sufficient to meet the needs of today's forces and their beneficiaries, and will not be sufficient to meet the needs of the future," said the draft report delivered by Vice Adm. Donald Arthur, the Navy's surgeon general.
That's a dry-sounding indictment from the group that came to Fort Carson last January as part of its tour of more than 30 military bases, where members interviewed soldiers, sailors, airmen and Marines. Fort Carson has been under special scrutiny during the past year after Sen. Barack Obama, D-Ill., and other senators asked for a congressional investigation into complaints that Fort Carson soldiers were not getting needed mental health care or were being punished for disciplinary problems caused by post-combat stress.
While Army officials at Fort Carson have expanded the mental health screening program for soldiers, Obama and eight other senators toughened their position this month by asking for an investigation by the General Accountability Office, the investigative arm of Congress.
And if that weren't enough, the Pentagon's long-established task force that reviews troop morale and mental health released its latest review last Friday, looking at troops who served in Iraq last year. Its conclusions were much the same: mental health problems, suicides, and family problems worsened among troops who have made multiple deployments to Iraq.
At least Fort Carson wasn't singled out in the Pentagon task force reports for criticism.
"That's consistent with what (Sen. Ken Salazar) has been saying for months, " a spokesman for the Colorado Democrat said Friday. "The Defense Department and the Veterans Administration are not adequately equipped to deal with the volume of these cases. This is a systemwide problem, not a problem at Fort Carson alone."
Salazar and Sen. Wayne Allard, R-Colo., sent a letter to the GAO last week asking that any investigation of Fort Carson look at mental health issues throughout the Defense Department.
Thus far, no one has said Fort Carson's treatment system is the worst - not even the Veterans for America group that has interviewed soldiers at the Mountain Post and provided case information to Obama and other critics. The group, made up of veterans, argues that in the crush to keep soldiers in the Army and available for redeployment, some Fort Carson soldiers are not getting the treatment they need or not having their post-combat stress recognized as a cause of disciplinary problems.
Fort Carson officials have defended their system for screening and treating soldiers suffering from post-combat trauma. They cite statistics on how many cases of Post-Traumatic Stress Disorder they have diagnosed, treated or referred to a medical review board for discharge. They will get to defend it again, as a Senate delegation is scheduled to visit the post later this month.
All of the task forces have identified a common problem in the military culture - soldiers and Marines are reluctant to ask for mental health care if they have any plans to stay in the military because they fear they will be seen as weak or it will damage their careers.
According to the 2006 survey of troops in Iraq:
59 percent said they feared their unit would view them differently if they asked for mental health care
55 percent said they would be viewed as weak
54 percent said their unit would lose confidence in them
36 percent feared it would hurt their career
And nearly 40 percent of soldiers and Marines said they did not trust mental health professionals.
VA urged to improve testing, compensation for veterans with stress disorder
WASHINGTON (AP) — The surge in the number of veterans suffering post-traumatic stress disorder requires development of better tests to evaluate affected personnel and determine how best to compensate them, a panel of medical experts said Tuesday.
http://www.timesrecordnews.com/trn/local_news/article/0,1891,TRN_5784_5526336,00.html
"As the increasing number of claims to the VA shows, PTSD has become a very significant public health problem," said Nancy Andreasen, chair of the committee that prepared the report.
"Our review of the current methods for evaluating PTSD disability claims and determining compensation indicates that a comprehensive revision is needed," said Andreasen, head of the psychiatry department at Carver College of Medicine, University of Iowa.
Claims increased from 120,265 in 1999 to 215,871 in 2004 and payments jumped from $1.72 billion to $4.28 billion in the same period, a combined committee from the Institute of Medicine and National Research Council said.
While the largest share of claims is still coming from Vietnam War veterans, there are expected to be many more claims in future from personnel who served in the first Gulf War and in the current conflicts in Iraq and Afghanistan, the panel said.
But the Veterans Affairs Department uses only crude criteria for rating disabilities due to mental illness and is not consistent for relapsing conditions, according to the report, which had been requested by the VA.
The panel urged the VA to develop new criteria based on the diagnostic standards of the American Psychiatric Association and to establish certification programs for workers who deal with PTSD claims.
The panel said the VA should base compensation decisions on how greatly PTSD affects all aspects of a veteran’s daily life, not just his or her ability to be gainfully employed.
The report also noted that PTSD can be triggered by trauma other than combat, such as sexual assault. Female veterans are less likely to receive compensation for PTSD, which may in part be due to the difficulty of substantiating exposure to traumatic events unrelated to combat, including sexual harassment or assaults that occurred during service, the report said.
Migraines may be sign of post-traumatic stress for Iraq veterans
http://www.news-medical.net/?id=24727
Soldiers returning from combat in Iraq who have migraine headaches are more than twice as likely to also have symptoms of post-traumatic stress, depression or anxiety than soldiers who do not have migraines, according to research presented at the American Academy of Neurology's 59th Annual Meeting in Boston.
The study involved 3,621 United States Army soldiers who were given a health screening questionnaire within 90 days after returning from one year of combat duty in Iraq. A total of 2,167 of the soldiers, or 60 percent, completed the questionnaire. Of those, 19 percent screened positive for migraine headaches, 32 percent screened positive for depression, 22 percent screened positive for post-traumatic stress disorder, and 13 percent screened positive for anxiety.
The researchers found that 50 percent of those with migraine also had depression, compared to 27 percent of those without migraine. A total of 39 percent of those with migraine also had post-traumatic stress disorder, compared to 18 percent of those without migraine. And 22 percent of those with migraine also had anxiety, compared to 10 percent of those without migraine.
"Previous studies in non-military populations had revealed a higher prevalence of certain psychiatric conditions, such as depression and anxiety, among people with migraine," said study author Maj. Jay C. Erickson, MD, PhD, of Madigan Army Medical Center in Tacoma, WA. "We hypothesized that there would be a similar relationship between migraine and psychiatric conditions in soldiers. The precise reasons for such an association are not fully understood, but may be related to similarities in the mechanisms underlying migraines and some psychiatric disorders."
The study also found that those with migraine and depression also had more frequent headaches than those who had migraine with no depression , an average of 3.5 headache days per month for those with depression compared to 2.5 days per month for those with no depression. The findings were similar for those with migraine and post-traumatic stress disorder.
"These findings should alert health care providers, especially those affiliated with the military or veteran health care systems, about the frequent association of migraine headaches and psychiatric conditions in soldiers returning from deployment," Erickson said. "We recommend that health care providers who evaluate combat veterans for headaches perform mental health screening in order to ensure that psychiatric disorders are identified and properly treated. All soldiers returning from deployment presently undergo mental health screening."
A Dose of Virtual Reality
http://www.businessweek.com/technology/content/jul2006/tc20060725_012342.htm
Doctors are drawing on video-game technology to treat post-traumatic stress disorder among Iraq war veterans.



Dr. Dennis Wood takes patients on what some might consider an odd journey. He starts off leading them to a military compound in Fallujah, Iraq. He then guides them through an Iraqi marketplace before they accompany a patrol through Iraqi homes. And if he thinks they're up to it, he may even take them onto a battlefield, in the midst of explosions and aircraft flying overhead.
But neither Wood nor the patients is anywhere near Iraq. The therapeutic conflict is part of a virtual reality program developed at the Virtual Reality Medical Center in San Diego and funded by the Office of Naval Research (ONR). It's designed to help personnel returning from the wars in Iraq and Afghanistan cope with so-called acute post-traumatic stress disorder, or PTSD. Brought about by distressing experiences like those in war, PTSD can lead to flashbacks, other psychological ailments, and social problems.
COPING STRATEGIES. A therapist at the Naval Medical Center in San Diego, Calif., Wood monitors patients' heart and breathing rates and even how much they're sweating to see the effect of the virtual environments. The aim is to get patients to draw on their meditation training to regain perspective—and stay calm—when a stimulus causes an emotional response. "The idea being to be in the high-stimulus environment for a long period of time, maintaining low psycho-physiological arousal," Wood says. "The person then can take that learning in the therapeutic environment and transport it out or generalize it to day-to-day life."
There may be a great need for PTSD therapy among veterans of the war in Iraq. A 2004 study published in the New England Journal of Medicine estimates that PTSD afflicts about 18% of the troops in Iraq. That study took place early in the war, and the figure now may be higher, says Emory psychiatry professor Barbara Rothbaum. She co-owns Virtually Better, a virtual reality treatment company that has received funding from the ONR to develop and test a version of the therapy. "Things over the past few years have gotten even worse," she says. "I hope we're wrong, but I think everybody's expecting probably a higher rate of PTSD." There are currently 127,000 troops stationed in Iraq, according to the U.S. Defense Dept.
Petty Officer Second Class Armando Guerrero has just completed his third session under the program at the Naval Medical Center. It was his first to incorporate the full virtual reality treatment. A recalled reservist from Texas, Guerrero worked as an equipment operator in the Navy's construction battalion in Iraq. He hopes the virtual reality treatment will help him cope. "Some of it does resemble the real Iraq," Guerrero says. "The only thing they need is the smell."
SUPPLEMENTAL HELP. Soon, therapies like the one he's taking will even have that. Guerrero was part of a program for noncombat personnel. But it's part of a larger $4 million project funded by the ONR that began in April, 2005, and is designed to test virtual reality treatments for a variety of personnel. One treatment incorporates not only smell but feel as well. A version of the treatment for returning combatants is just now being distributed to various facilities, including academic institutions and military installations such as the Naval Medical Center in San Diego.
Rothbaum is conducting research that she hopes will make that version even more effective. In August, researchers at Emory University will begin studying the effects of combining the virtual reality PTSD treatment with a drug shown to augment virtual reality therapy. The drug, called D-cycloserine, was tested in a 2004 study by Emory researchers and significantly enhanced the therapy treating acrophobia, or fear of heights. "After treatment, and then again three months later, the people who got the D-cycloserine reported less fear," Rothbaum says. "After two pills and two sessions, they were doing better than the people who got the placebo." The Emory research project is funded by the National Institute of Mental Health and uses the Iraq treatment developed by Virtually Better and the Institute for Creative Technologies at the University of Southern California.
Rothbaum and other doctors treating PTSD are drawing on lessons learned from the Vietnam War. Virtually Better developed a Virtual Vietnam VR therapy program in 1997 to help Vietnam war vets struggling with PTSD. A congressionally commissioned survey of Vietnam veterans released in 1990 found 30.9% of male and 26.9% of female Vietnam vets had a lifetime prevalence of PTSD.
SENSORY OVERLOAD. But Rothbaum hopes treating soldiers from the current conflicts soon after their combat experience can prevent PTSD later in life. "It's decades after Vietnam," she says. "There's been so much disruption in people's lives. What we're hoping is, if we can get people closer in time to when they served in Iraq, we can treat the PTSD and get them feeling better."
Makers of VR treatments also make heavy use of computer game technology. Some have incorporated graphical and audio elements from a military training video game called Full Spectrum Warrior and combined them with newly developed graphics and sound to create the virtual reality treatment environment. "Looking at the video-game industry in general as a source of help and innovation is at least one of my big goals," says Commander Russell Shilling, program manager at the Office of Naval Research. Shilling is no stranger to the games industry. He was the sound designer for the U.S. Army's recruitment game America's Army.
Full Spectrum Warrior's designers have taken their game and meshed it with the VR hardware experience of Virtually Better to make an emotionally stimulating program incorporating the sounds, visuals, feelings, and smells from Iraq. "Evoking emotion in a simulation, even in training, is a fairly new idea for us," says Shilling. The simulation uses VR headsets to immerse the patient in the world. It also uses bass shakers that rumble the patient's seat and a smell machine that can create scents.
REALITY BITES. The point is not to retraumatize the patients but to allow the individuals to cope with painful experiences. "The concept here is that by doing this in a very modestly paced manner, the person feels little bits of anxiety as they go through this, but not at a level that overwhelms them," says Albert "Skip" Rizzo, a research scientist at the Institute for Creative Technologies. "Eventually they're actually in the Humvee, driving down the road, and children are by the side of the road, and an IED (improvised explosive device) goes off and there's body parts everywhere." The institute has gotten feedback from therapists and even soldiers in Iraq to develop more accurate versions of the program, he says.
Even with less-than-perfect graphics, PTSD patients respond well to simulations, says Hunter Hoffman, who is leading another ONR-funded project at the University of Washington. "They come out saying that was really powerful, whereas someone who doesn't have PTSD might be less impressed with it," he says. "The patient is actually bringing a lot to that world. They may remember seeing things that aren't actually shown."
Hoffman says his program has gotten off to a slow start due to a very involved training process for therapists. "We're going to go gangbusters once we get started," he says. "We've got our software ready, and we certainly have soldiers."
Soldiers Face Obstacles to Mental Health Services
http://www.npr.org/templates/story/story.php?storyId=6575431
Post-Traumatic Stress Treatment Costs Soar
http://www.npr.org/templates/story/story.php?storyId=5441927
U.S. Department of Veterans Affairs has watched the amount of money paid to cover treatment for claims of Post Traumatic Stress Disorder (PTSD) rise significantly in the last five years. Some researchers believe veterans who aren't eligible for PTSD compensation are claiming disability. But efforts to redefine PTSD is alarming some veterans' advocates.
Soldiers' crimes
http://www.veteransforamerica.org/index.cfm/Page/Article/ID/9620
SAN JOSE, Calif. - One night last July, Iraq war veteran Nicholas Rusanoff followed his neighbor, Peter Losher, into the parking garage of their apartment complex.
Rusanoff was breathing heavily. His eyes were wide open, and his hands were clasped behind his back. He demanded the keys to Losher's Volkswagen Jetta, and Losher quickly complied.
"As I was getting out of the vehicle, he looked at me and said, `You're not Iraqi, you're not Iraqi,'" Losher later testified at a court hearing. "I said, `No, I am not.'"
Losher said he could hear Rusanoff screaming in pain as he drove away.
Rusanoff, 25, is one of a growing number of soldiers who have returned from the war in Iraq only to become entangled in the criminal justice system at home.
Some have committed minor offenses; others are facing serious charges of domestic violence and even homicide. Many are struggling with psychological issues as they try to adjust to civilian life.
No one tallies the number of soldiers and veterans in the criminal justice system, so it's impossible to know how many criminal cases involving Iraq war veterans are pending nationwide. But as the war entered its fifth year this month, the conflict is coming home in yet another painful way.
Among the incidents:
In February 2004, a former Marine broke his girlfriend's neck and left her to drown in the bathtub of her Oceanside, Calif., apartment. The couple became romantically involved while deployed in Iraq.
In July 2005, a 19-year-old Fort Lewis, Wash., soldier who earned a Purple Heart in Iraq murdered his wife. She was stabbed at least 71 times.
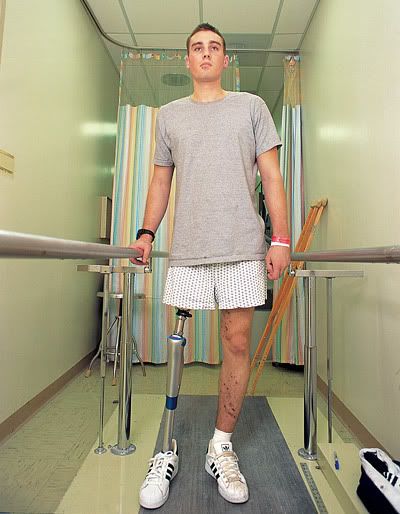
In February, a 24-year-old Pennsylvania man who lost his leg in Iraq was accused of setting a mobile home on fire while a family was inside, then choking a firefighter who responded to the blaze.
"It's a brazen indicator, as Iraq war veterans enter the criminal justice system, that there are untended psychic wounds," said Jim Barker of San Jose, Calif., a Vietnam veteran who worked as a psychiatric clinician at the Veterans Administration Hospital in Palo Alto until retiring in 2005. "The coordination of care needs to be sharpened up."
Military officials and veterans advocates emphasize that the overwhelming majority of returning soldiers are law-abiding citizens who have not run afoul of the law. And psychiatric clinicians such as Barker point out that most people with mental health issues do not commit crimes.
In recent weeks, however, concern about the care returning soldiers are receiving has intensified. Articles in the Washington Post about conditions at Walter Reed Army Medical Center triggered congressional hearings. Three top Army officials have resigned, and the White House has ordered a review of military and veterans hospitals.
There are only two known felony cases in the Bay Area in which Iraq war veterans are defendants. The second case, also in San Mateo County, involves Yodi Shembo, a 24-year-old Marine who allegedly attacked a police officer at San Francisco International Airport last October. Shembo, who had recently returned from a full tour in Iraq, had torn off his shirt and was yelling at other passengers.
"It's very clear that we are dealing with mental health disorders," said Steve Wagstaffe, San Mateo County's deputy district attorney. "We had a lot of post-Vietnam cases in the late 1970s, and we're going to begin to see that here."
Rusanoff faces charges of carjacking and grand theft auto; his jury trial is scheduled to begin June 25. Shembo faces charges of assault with force and assault on a police officer; his next hearing is scheduled for April 9.
Some Iraq war veterans who have landed in jail have already been diagnosed with post-traumatic stress disorder, or PTSD. Others may have mental health issues that predated their deployment. Despite stepped-up outreach efforts, clinicians acknowledge that thousands of Iraq and Afghanistan veterans struggle in isolation and are reluctant to seek treatment, often "self-medicating" with alcohol and drugs.
Advocates for veterans say the criminal cases are evidence that returning soldiers are not receiving the mental health care they need.
"This new generation of veterans has experienced combat very recently, and it's very raw," said Dick Talbott, who oversees 31 community-based vet centers in California, Oregon, Hawaii and Guam. "They are going to need more intensive and frequent counseling from us, a greater level of care and more staff."
The Department of Defense, however, says it is aggressively reaching out to troubled soldiers, from placing mental health units in the field in Iraq to conducting mental health screenings three to six months after soldiers return home.
But those who work closely with Iraq war veterans say that while outreach has improved, much more is needed.
Steve Robinson, director of veterans affairs for Veterans for America, says it is critical to determine what mental health care any veteran charged with a crime has received. "If a veteran gets a DUI or is charged with domestic violence or murders his wife, I want to know: What kind of mental health treatment did he get before he separated from the military?" Robinson said. "What kind of treatment is he getting from the VA? Did we do everything we could to help him reintegrate into society? And the answer is usually no."
Some clinicians talk about a phenomenon known as "pancaking" - when a veteran's life collapses. The downward spiral often includes alcohol or drug abuse, a fractured family, joblessness and homelessness.
"If you think that society has betrayed you, if you don't have a job, if your family has broken up, if you can't get VA health care or benefits, or if you don't have a place to live, then you may get involved in petty crime to make ends meet," said Paul Sullivan, a former VA project manager who testified to Congress this month.
While most of the draftees in Vietnam were young and single, "a lot of the guys who have gone to Iraq are older, married and have kids," said Barker, an Army intelligence specialist in the Vietnam war. "Now you have a family in crisis, not just an individual in crisis."
Wagstaffe, San Mateo County's deputy district attorney, said his office needs to hold soldiers and veterans, like any other criminal suspect, accountable because the overriding concern is public safety. Still, he said, their service in Iraq and psychological issues will be taken into account during sentencing.
"We are looking at these cases differently than the person committing a carjacking because they just want a car," Wagstaffe said.
In Massachusetts, the Norfolk County District Attorney's Office has launched an unprecedented effort to prepare police officers and others to interact with soldiers and veterans who may pose risks to themselves and others. Mindful that more than 1.6 million Americans have now served in Iraq and Afghanistan, the office is training police and probation officers, firefighters and emergency medical technicians on the signs of PTSD.
PTSD "manifests itself in many ways, and we want our first-responders to recognize this," said Norfolk County District Attorney William Keating. "It's not a get-out-of-jail-free card, but if a veteran has a brush with the law, we need to help him."
Keating's uncle struggled with PTSD after serving in World War II, and that inspired him to launch the program. His office has created a 10-minute training video, available on YouTube, in the hope that increased public awareness will reduce veteran-related crime.
"As the trickle of soldiers coming back from Iraq becomes a flood, more of these kinds of cases are going to happen," Keating said. "Helping veterans assimilate and get the kind of treatment they need - even if they are in the criminal justice system - is the least we can do."
---
CRIMES INVOLVING RECENT VETERANS
_Wardell Nelson Joiner, 25, was convicted of murder after breaking Lance Cpl. Vanessa Messner's neck and leaving her to drown in a bathtub in her California apartment in February 2004. The couple met at Camp Pendleton and became romantically involved while deployed to Iraq. Joiner, a former Marine, was sentenced to life in prison without the possibility of parole.
_Brandon Bare, a 19-year-old Fort Lewis Army soldier, was found guilty of premeditated murder and indecent acts for the July 12, 2005, murder of Nabila Bare, his 18-year-old wife. She had been stabbed at least 71 times, and a pentagram was carved into her stomach. A military panel sentenced Bare to life in prison.
_Salvatore "Sam" Ross Jr., 24, of Fayette County, Pa., is accused of setting a mobile home on fire in February and then choking a firefighter who responded to the blaze. Ross lost his left leg while serving in the Army in Iraq.
_In December 2005, Jeff Lehner, 40, a former Marine sergeant who served in Afghanistan, shot and killed his elderly father, then killed himself in Santa Barbara County. He had been in counseling for combat-related post-traumatic stress disorder.
_Jared Terrasas, 24, a former Camp Pendleton Marine, faces charges that he abused his 7-month-old son so severely that he died. Terrasas served two tours of duty in Iraq before he was discharged following the baby's death in October 2005.
_Johnny Lee Williams Jr., 24, a former Marine who served in Iraq, kidnapped a clerk at a Texas Wal-Mart in January 2005. Megan Leann Holden, 19, was later found shot to death in a ditch. Williams pleaded guilty to murder and was sentenced to life in prison.
PTSD & Parkinson's Disease: Longer Version







![Brotherhood" (2006) [TV-Series]](http://photos1.blogger.com/x/blogger2/1421/379621144723082/211/z/425926/gse_multipart33129.jpg)



No comments:
Post a Comment